
Six common myths contribute to ongoing misunderstanding and stigma, despite the established facts about epilepsy.
Image: KOS Chiropractic Integrative Health/pexels
Epilepsy is one of the oldest and most misunderstood medical conditions in the world. Affecting over 50 million people globally, this neurological disorder transcends age, culture and geography, yet continues to be shrouded in stigma and silence.
International Epilepsy Day, observed on February 9, is more than a date on the calendar; it’s a call to action, a chance to dismantle myths, and an opportunity to normalise the lived experiences of those affected.
Epilepsy is more common than many realise, impacting 1 in 100 people in South Africa alone and millions worldwide. Yet, fear and misinformation distort its public perception.
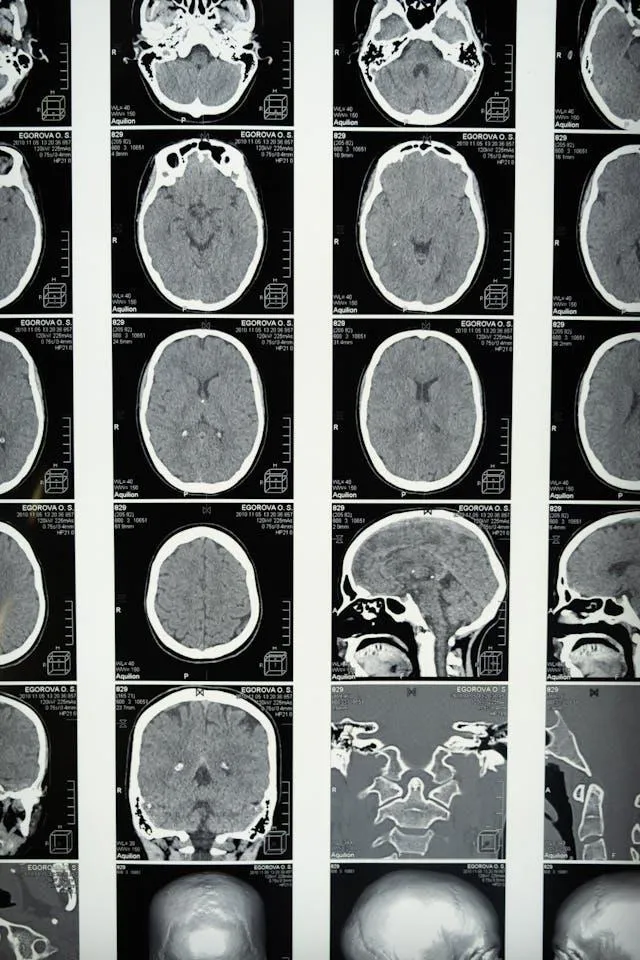
At its core, epilepsy is a chronic condition characterised by recurrent seizures caused by abnormal electrical discharges in the brain. These seizures can range from subtle moments of blank staring to dramatic convulsions. Importantly, one isolated seizure does not equate to epilepsy; it’s defined by two or more unprovoked seizures.
The condition is not contagious, nor is it a mental illness. Epilepsy is a physical neurological disorder, yet misconceptions often lead to harmful stereotypes. These myths don’t just perpetuate stigma; they actively harm those living with epilepsy.
In South Africa alone, epilepsy impacts about 1 in 100 people, emphasising the need for stronger awareness initiatives.
Image: cottonbro studio/pexels
Despite the factual landscape of epilepsy, six common myths perpetuate misunderstanding and stigma. An initiative by Fedhealth seeks to debunk these fallacies:
Myth 1: Epilepsy is rare
Fact: Far from it. Epilepsy affects people across all demographics, yet societal stigma often drives individuals to hide their condition. This silence perpetuates the false notion that epilepsy is uncommon.
Myth 2: All seizures look the same
Fact: Seizures vary widely. While some may involve convulsions, others are barely noticeable, like brief moments of confusion, repetitive movements, or a sudden sense of déjà vu. Misunderstanding these subtle signs often delays diagnosis and treatment, worsening outcomes.
Myth 3: Epilepsy is a mental illness
Fact: While epilepsy can take an emotional toll, it’s a disorder of the brain’s electrical activity, not a mental health condition. Understanding this distinction is vital to combating stigma and ensuring those affected receive proper care.
Myth 4: You should restrain someone during a seizure
Fact: Restraining someone can cause injury. Instead, focus on clearing the area of hazards, cushioning their head, and gently turning them onto their side once the seizure subsides. Always seek medical help if the seizure lasts longer than five minutes or if it’s the first known seizure.
Myth 5: Epilepsy can’t be treated
Fact: While not always curable, epilepsy is highly manageable. Anti-epileptic medications help the majority of sufferers control their seizures, enabling them to live full, independent lives.
Myth 6: People with epilepsy can’t work or live independently.
Fact: With the right medical care and support, most people with epilepsy can lead typical lives, thriving at work, school, and home. South African labour laws even protect individuals with epilepsy from workplace discrimination.
Living with epilepsy is more than just managing seizures; it’s navigating a complex emotional and social landscape. Anxiety, depression, and fear of judgment are common companions for those with epilepsy.
Many feel the weight of societal misunderstanding and experience isolation or discrimination.
Environmental and social factors also play a crucial role in how the condition is managed. In low- and middle-income countries, lack of access to medical care, delayed diagnoses, and harmful traditional beliefs often exacerbate the challenges.
Misconceptions like epilepsy being caused by witchcraft or possession can lead families to seek spiritual healing instead of medical treatment, delaying care and increasing risks.
But there is hope. Education, support, and advocacy are breaking down barriers. From improved access to anti-epileptic medications to workplace accommodations, progress is being made.